PROS
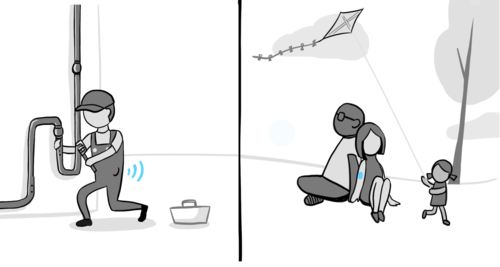
Almost fingerstick-free
Two of the three sensors available don’t require finger sticks! You still want to have a meter with you, in case, but you won’t need it hardly as much.
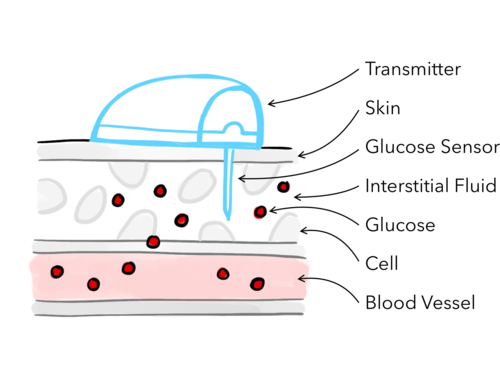
Prevent lows and highs before they happen
A CGM shows you which direction your blood sugar is headed and how fast. Some types will alarm during the day or night to help alert you when you have a low or high blood sugar.
Notice Patterns and Adjust Insulin Having sensor data gives you the ability to see patterns that happen over time. You can look at it with your doctor to adjust insulin, food and exercise routines.
CONS
Alerts and alarms
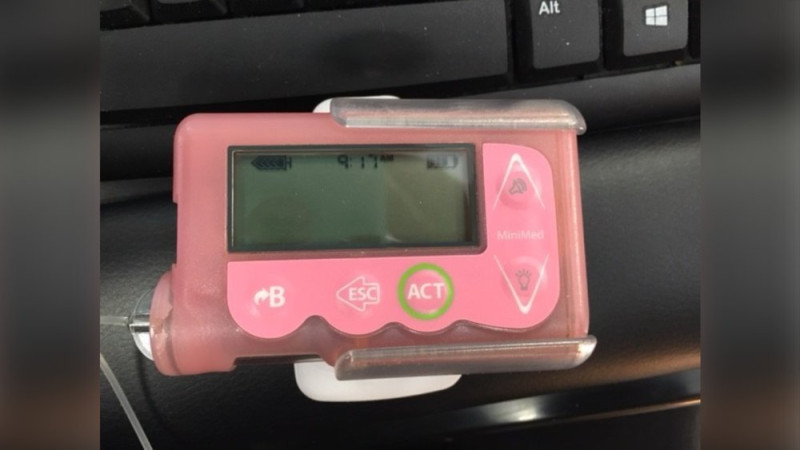
Some people get overwhelmed with too many alerts sounding from their devices. You can tailor them to fit your needs and wants, or turn them off entirely (except the emergency low alarm).
Attachment to devices
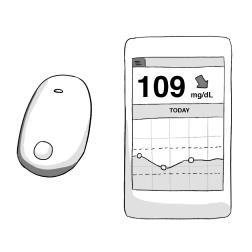
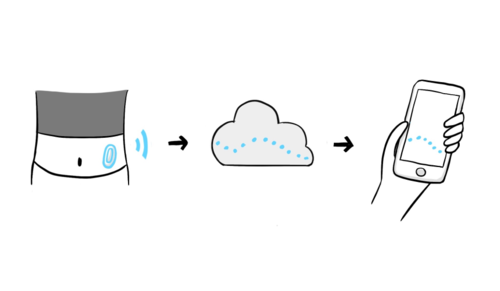
Wearing a CGM means you will have a device on your body at all times. They’re all waterproof and very durable. Some CGMs have receivers, and others can be linked to a smartphone, which can reduce the number of devices you have to carry!