Device Combo

What type of diabetes do you have?
T1D
What is your primary physical activity, exercise, or sport?
Running
If you participate in other physical activities, exercises, or sports, what are they?
Weightlifting, gymnastics, and stroller runs with my toddler.
What devices do you use to track your physical activity:
Apple Watch, considering getting an Aura Ring
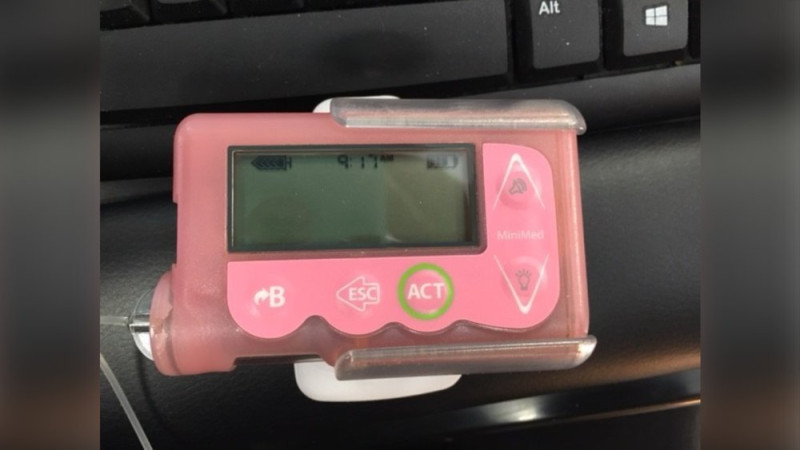
What devices do you use to manage your diabetes?
I currently use iAPS, but have used Loop, a DIY AID system, for the past 6 years. I use either a Dexcom G6 or a Dexcom G7 CGM.
Why did you choose your devices?
I really enjoy using automated insulin delivery to relieve some of the mental burden of having to live with T1D. Because the systems can automatically increase and decrease insulin doses in response to glucose levels, I can think about diabetes a little bit less.
What challenges do you have around diabetes and exercise, and how do you overcome them?
Over the years, I have had to think a lot about exercise and type 1 diabetes. I am very insulin sensitive, so if I have even a small amount of insulin on board before starting an aerobic activity, my blood sugar levels will drop significantly. I usually have to plan 2 hours in advance, and I try to avoid taking insulin or eating 2 hours prior to activity unless it is a low carb or carb free snack. I really like high-protein snacks prior to activity.
What would you tell someone considering the same devices that you use?
I think the automated insulin delivery systems can really help take a lot of the guesswork out of managing type 1 diabetes.
What is your favorite low snack?
I use juice boxes or glucose gel. They work quickly so I can get back to work!
Do you have anything else that you want to share?
Exercise has always been one of the most challenging parts of managing type 1 diabetes. There are so many complex factors that can influence blood sugar levels, including diet, type of activity, stress level, recent hypoglycemia, recent hyperglycemia, insulin absorption, how many days you have had your infusion site in place, etc. I also check fingersticks during exercise, because when my blood sugars are dropping quickly, the CGM readings may lag behind my actual glucose values. I always trust my instincts, and if I feel like I'm getting sleepy all of a sudden while exercising, I know to double-check to be sure my blood sugars aren't dropping. I also had to manage exercise during my most recent pregnancy, and I had to change my strategy based on the hormonal changes that occurred each trimester. In the first trimester, I was very sensitive to insulin and had to reduce my insulin on board prior to activity more than ever before in my life. I would usually disconnect my pump an hour ahead of activity and make sure any insulin on board was negative. Inevitably I would still have hypoglycemia and need to treat it with quite a few juice boxes. Because I had to take off my pump for 2 hours, and because of the stress hormones I accumulated during activity, my blood sugars would spike immediately after activity, so I would give myself 1-3 units of rapid-acting insulin as soon as I finished exercising to make up for the insulin I was not receiving during the activity. This is not so unusual, as I do this on a regular basis when I am not pregnant, but the amounts changed slightly. During the second trimester, I had fewer lows with activity and had to reduce my insulin doses less than compared to the first trimester. During the third trimester, with increased insulin resistance, I never reduced my insulin doses prior to activity and actually had to give insulin during activity, which was a completely new scenario for me. I did not have post-exercise hyperglycemia because I had not reduced my insulin doses prior to/during activity, which was great! It was much easier to manage activity and I was not longer afraid of lows.
Ask the Expert Wisdom
On the timing of insulin adjustments
before exercise:
"To avoid hypoglycemia during exercise with automated insulin delivery systems, it's generally recommended to set a higher glucose target 1-2 hours before planned activity to account for the time it takes to lower insulin levels in the body." — Dessi Zaharieva, PhD
More Wisdom
This disease is frustrating as it is, but using a pump/meter helps to simplify just one part of it.
Betsy

I Didn't Decide To Get A Pump Until My Doctor Said To Me, "You Are Giving Yourself The Best Care Possible While On Injections. If You Want Your Numbers To Get Better, The Type Of Technology You're Using Has To Change.
Chelsea

I really don't like having to wear two sites, but I love that my pump tailors my basal rate.
Anne