PROS
Casi sin puntero
¡Dos de los tres sensores disponibles no necesitan puntero! Por si acaso, no te vendrá mal llevar un medidor, pero apenas lo necesitarás.
Evite las bajadas y subidas antes de que se produzcan
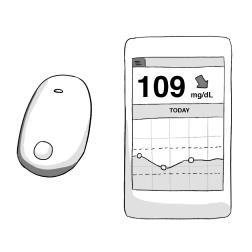
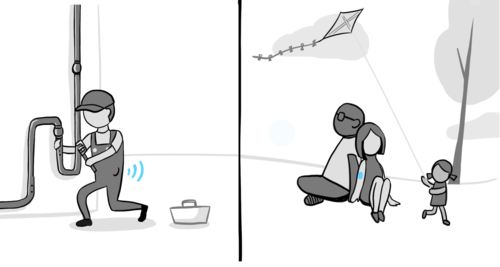
Un MCG le muestra en qué dirección se dirige su glucemia y a qué velocidad. Algunos modelos emiten una alarma durante el día o la noche para avisarle cuando tiene un nivel bajo o alto de azúcar en sangre.
Observe los patrones y ajuste la insulina Disponer de los datos de los sensores le permite ver los patrones que se producen a lo largo del tiempo. Puedes consultarlos con tu médico para ajustar las rutinas de insulina, alimentación y ejercicio.
CONS
Alertas y alarmas
Algunas personas se sienten abrumadas por el exceso de alertas que emiten sus dispositivos. Puede adaptarlas a sus necesidades y deseos, o desactivarlas por completo (excepto la alarma baja de emergencia).
Fijación a los dispositivos
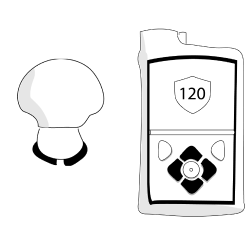
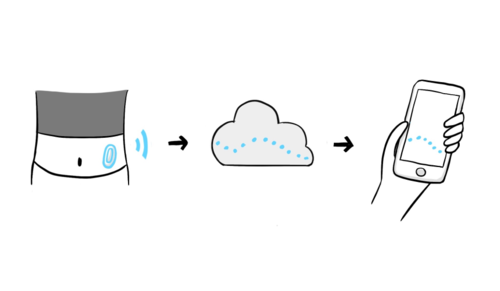
Llevar un MCG significa que tendrá un dispositivo en el cuerpo en todo momento. Todos son resistentes al agua y muy duraderos. Algunos MCG tienen receptores y otros pueden vincularse a un smartphone, ¡lo que puede reducir el número de dispositivos que tienes que llevar encima!